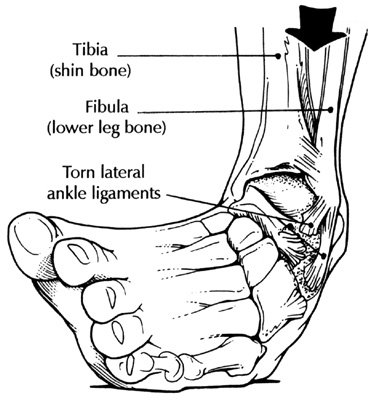
In my last blog, I discussed the importance of ankle
rehabilitation and continued mobility in maintaining balance, especially in the
elderly population. I also briefly mentioned how poor posture in the elderly
can often contribute to the high prevalence of falls. Here, I will discuss this
in more detail.
As I mentioned previously, a common trait in the elderly is
their shuffled walking pattern and stooped posture, both significant
contributing factors to the high incidence of falls in older adults.
Many factors play a role in contributing to the stooped
posture seen in the elderly:
·
Reduced eyesight, causing people to look down at
their feet to see where they are going
·
Weakened abdominal muscles
·
Weakened upper back and neck muscles
·
Limited arm swing
·
Shuffled walking due to reduced hip flexion,
poor balance and limited ankle flexibility and stability – discussed previously
Poor eyesight will not be dealt with here, but it is
important to remember that even if you see a step and it is right in front of
you, chances are it will be too late for you to correct your step before tripping.
Rather keep your head up, and focus your eyes about 3 metres ahead of you on
the ground. This way, you simply have to drop your eyes slightly and you have
time to step appropriately before tripping over any uneven surface ahead of
you.
Abdominal strengthening exercises should be done regularly
in order to maintain core strength, as this keeps one’s posture upright. When
you walk, pull you navel in towards your spine, keep your hips underneath your
shoulders and walk with long strides, striking the ground with the heel first.
Pretend you have a piece of string attached to the top of your head that is
gently pulling you up as you walk.
It is very important to maintain strength of the upper back
and neck muscles because it is weakness in these muscles that causes the head
to drop and the typical stoop to develop. This causes one’s centre of gravity
to shift forward, contributing to falls. In order to prevent this, one must
keep looking straight ahead and keep the chin tucked in by gently pulling the
head back. The upper back muscles can be strengthened by squeezing the shoulder
blades together and releasing 10 times and then holding the squeeze for 10
counts at a time. This can be done while waiting in a queue or watching TV.
Finally, arm swing must be maintained to keep balance and a
good stride length. As soon as one’s upper body stiffens, the rest of the body
does as well, resulting in a shuffle.
So, remember: walk tall, look ahead, keep the shoulders
back, swing the arms, lift the knees and feet, and strike the ground with your
heel first! J
Merry Christmas and may you all have a happy and healthy 2013! J